What’s in a pain rating? As health care providers, most of us ask the question, “what is your pain,” during each patient encounter; but why? What is the value of asking a patient’s pain rating? Is it helping your patients achieve optimal outcomes? I suspect not!
Pain is the most common reason for seeking health care services and most health care providers ask for their patient’s pain rating at the initial consultation and subsequent encounters. A survey of members of the American Pain Society (APS) demonstrated that 89% of members ask for pain ratings of most patients at the initial visit and 81% ask for pain ratings of most patients at subsequent visits.1 There are 164 million ambulatory physical therapy visits in the US each year for musculoskeletal disorders2, so imagine how often the question “what is your pain rating,” gets asked by physical therapists. Are you sick of this question? I bet your patients are too!
In this blog post, I will address the following:
- Understand the impact of asking your patient for a pain rating
- Using clinical reasoning to determine when it is appropriate to ask for a pain rating
- CMS and the Joint Commission stance on pain ratings
- Alternative options to measure progress
The impact of pain ratings
In 1996, the president of the American Pain Society, Dr. James Campbell, said in a speech,“if pain were assessed with the same zeal as other signs (vital) are, it would have a much better chance of being treated properly.” From this, the idea took hold that America was under-treating pain, and pain ratings became the 5th vital sign. With the incidence of pain and disability increasing and the ongoing opioid epidemic today, in the wise words of Patrick Wall, “If we are so good [at treating and measuring pain], then why are our patients so bad?”
Based on the neuroscience of pain, it is suggested that pain ratings have low clinical utility, largely because pain is complex and is an individualized experience that cannot be assessed accurately or reliably using a 10 point scale. Since pain is a subjective report, there is no way to validate a patient’s perception of their pain rating. The research is overwhelmingly clear that pain intensity ratings and disability do not correlate, nor does pain and the health of tissues. In regards to language, the major concern regarding pain ratings is that the word “pain” is a very provocative word and might be a significant source for firing up the pain neuromatrix (the unique pattern of brain activation in response to a threat that gives rise to the sensation and experience of pain). 3 In fact, with the advent of pain science and the use of advanced brain imaging, we now know that asking patients over-and-over about their pain might in fact increase pain ratings. 4 So, hopefully, this gives pause to the idea that collecting pain ratings is essential with every patient at every visit. It is also important to reflect on if you, as a health care provider, are doing more harm than good for your patients by asking this question.
When is it appropriate to ask for a pain rating?
Having just discussed the potential negative impact of asking pain ratings, is there ever a time where it is appropriate to ask for a pain rating? The old saying goes, don’t throw the baby out with the bathwater, which suggests that we likely should not allow our pendulum of thinking to shift too radically, or should we? Many of the manual therapy approaches to treating pain operate on the “find it, fix it” model, whereby the clinician identifies an impairment, applies a treatment, and re-assesses the impact of that treatment. Often that assessment is done by asking the patient a pain rating before and after the treatment is applied. As an example, for a patient with neck pain when turning their head to the left, the therapist may ask, what is your pain when you look to the left? The patient may identify it as a 6/10. The therapist then performs a treatment or guides the patient through treatment and the patient is then asked to rotate their head to the left again. The clinician will ask, what is your level of pain now? “It is a 3/10 (50% improvement).” A change in pain rating may indicate treatment success or the absence of an effect. This use of the pain rating question serves as a communication mechanism between the patient and the clinician and may help to guide clinical decisions.
So, when is it appropriate to use pain ratings as a communication mechanism to evaluate treatment success? Based on the work of Keith Smart, a patient’s pain can be classified into three “buckets:” nociceptive, peripheral neurogenic and central sensitization (now termed nociplastic).5–7 In the figure below, each “pain bucket” is accompanied by the most common signs and symptoms consistent with each pain mechanism.
When pain is of the nociceptive variety, it may be appropriate to use pain ratings as a communication mechanism with the patient to assess for treatment effect. This would make sense because the pain is proportional to the nature/mechanism of the injury, which often means there are low fear-avoidance beliefs and behaviors to pain. Further, there are known aggravating (turning head to the left) and easing factors (looking forward), which is what the clinician is attempting to affect with treatment. Clinicians should be cautioned against using pain ratings for those patients with primary peripheral neurogenic and/or nociplastic symptoms, largely because the pain experience is often more complex for these individuals, with an accompanying higher risk that asking about their pain will increase their pain.
In addition, asking patients with any type of chronic pain to rate it numerically can sometimes be an act of futility. We have all heard answers like, “20 out of 10,” and responses like this are difficult to work through. Clinicians might assume their patients are exaggerating, don’t understand the scale, or are potentially seeking more pharmacological or invasive treatments. Patients are often just trying to communicate, “this pain is HIGHLY distressing to me… I can’t even put a number on your stupid scale,” and continue to struggle to feel heard.
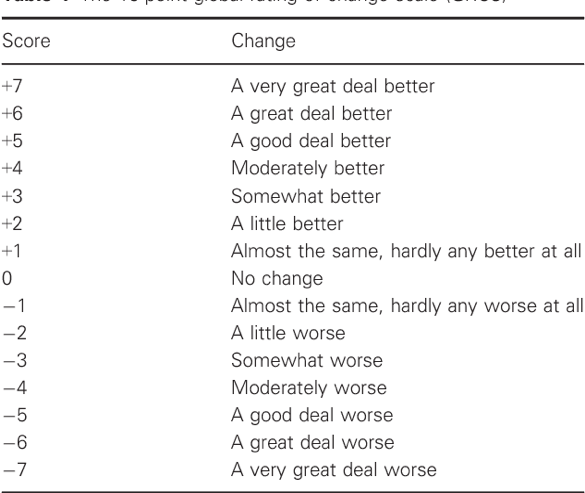
I challenge all clinicians to self-reflect and ask: is there a better way than using pain ratings to assess treatment response in patients with primary nociceptive pain? Could we instead ask patients during or after movements, “how did that feel?” or “what is the sensation in your neck like now?” If improvement is appreciated, the clinician could then ask, “What percent improvement?” (ie: “it is 50% better when I look to my left now”) or use the global rating of change scale.
CMS and the Joint Commission stance on pain ratings
In 2016, the American Medical Association recommended pain ratings to be dropped as the “fifth vital sign”8 as it might be part of the opioid epidemic, overly focusing on pain. In fact, The Joint Commission (JACHO), which oversees 21,000 health care organizations and programs in the US, has stated one of the biggest misconceptions is that pain ratings are required for all patients.9 In 2018 (further clarified in February 2020), newly published guidelines for pain assessment and management standards for hospitals were published by JACHO. These guidelines require that hospitals have defined criteria that are patient-specific to “screen, assess, and reassess pain.” Hospitals are also required to treat the patient’s pain or refer the patient for treatment, using pharmacological, non-pharmacological, or a combination of approaches. When clinicians determine the need for pain treatment, they must provide as an option at least one non-pharmacological pain modality. JCAHO stresses the need for a patient-centered approach to treating pain and the patient’s engagement in treatment decisions. They also comment that using numeric pain scales alone to monitor patients’ pain is inadequate. Additionally, the Joint Commission accreditation standards have never required clinicians to treat patients to “zero pain.” Finally, they stressed the importance of assessing how pain affects function and the ability to make progress toward treatment goals.10
You may be asking, what about the Centers for Medicare and Medicaid Services (CMS)? CMS requires documentation of a clinical assessment for the presence or absence of pain using a standardized tool and an accompanying follow-up plan if pain is present. Standardized tools are described as an assessment tool that has been appropriately normed and validated for the population in which it is used. Several example tools are listed (but not limited to) including several measures of functional ability or disability.
So, yes, you still must screen for, assess and document the presence or absence of pain in your patients. However, it is not required that you use the pain rating scale nor ask your patient about their pain several times throughout each visit. There is also a shift to focusing on function by assessing the impact of pain on a patient’s functional abilities. Assessing this may help shift the conversation and treatment focus from resolving pain to improving functional ability and quality of life. Regardless of what I propose based on current research and standards, all clinicians should comply with their employer, third-party payers, and governing bodies. If pain ratings are mandated, they need to be asked. In the next section, we will discuss how to ask them and alternate ways of assessing pain.
Measuring Pain and Progress
If you must ask for pain ratings
As mentioned in the previous section, many governing organizations require a pain rating, which ends up being a number written on a page or entered into an EMR. In line with modern pain science, clinicians should consider the timing and language when asking this question. It is not recommended that clinicians barge into the room and ask, “What’s your pain?” as the first thing they say. It could be argued that if a clinician first has a casual conversation with the patient regarding their life circumstances and then formally asks for a pain rating, it’s likely less provocative than asking it right upfront. Additionally, consider substituting other descriptors (i.e., ache) with the word pain. If their main concern is a “deep burning ache,” the “ache” should be rated, versus pain. It can be argued the word “ache” is less provocative than the word “pain.” Carolyn McMannus, an experienced physical therapist with a background in mindfulness, encourages working with your patient to re-label their pain as a “sensation.” The word sensation takes the judgment out of the experience your patient is having and may lead to less provocation. Consider this phrasing: “On a scale of 1 to 10, can you rate the sensation in your back?” Also, realize it’s not just the word pain that may be an issue, but even the pain scales using various facial expressions (Wong-Baker scales). For example, in some cultures smiling does not suggest feeling “good,” but potentially feeling embarrassed or angry.11.
Alternatives to pain ratings
If you are not required to collect pain ratings, this is fantastic news! Here are some other alternatives that will still allow you to screen for, assess and treat pain, and follow the guidelines set forth by JCAHO and CMS. First, I strongly encourage you to conduct a thorough examination to best understand the impact of pain on function and ensure that your patient belongs in your clinic. If your patient is experiencing pain, they are likely to share this information with you as it is often the reason they are seeking care. However, if you must, I recommend simply asking about the presence or absence of pain or a related synonym. If pain is present, your next question may be, “how is [descriptor] impacting your ability to do every-day activities?” You may also elect to ask about specific common activities, such as sleep, getting dressed, bathing, meal prep/eating, work activities, etc. This form of questioning will help you to understand the severity and intensity of your patient’s pain as it relates to their ability to perform daily living activities. Special questions can also be used to assess function, such as “If you had a magic switch and I could magically switch off this sensation in your back, what would you go and do?” This question will help you understand your patient’s deepest desires and what they would do if they were well again. Your treatment focus can now focus on function and helping your patient to get back to the activities they enjoy doing.
Motivational interviewing techniques, such as open-ended questions, can be incorporated into the patient interview to ascertain the “big picture” of pain and other associated symptoms a patient is experiencing. Consider using phrases such as: “Tell me about your symptoms and what concerns you most about them.” Questions like this avoid leading the patient in any specific direction. They may tell you about their pain, but also associated symptoms, such as mental fog, which actually may be troubling the patient more than pain itself.
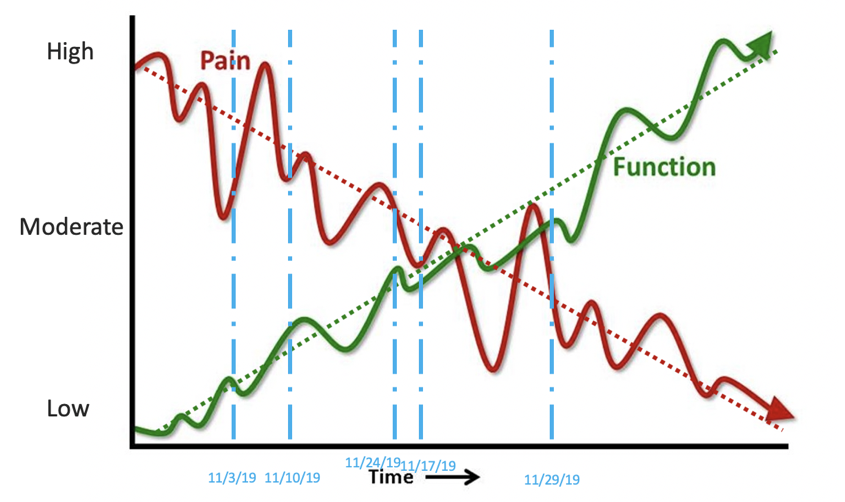
How will you measure baseline intensity and track progress? I recommend using functional outcome measures that are captured frequently (don’t let a month pass by before you administer these again!). One of the easiest validated measures to use is the Patient-Specific Functional Scale (PSFS), which is patient-centered and individualized to each patient. You can also consider several other more region-specific functional measures. For tracking progress, I recommend using the Global Rating of Change Scale, which measures the patient’s perception of change over time. You might also ask the simple question of “What percent recovered are you?” Finally, a neat graph that I personally use clinically is the Pain vs Function graph. This can be a great visual to demonstrate to patents that by focusing on function, pain is likely to decrease over time. Note that the lines are not straight lines; rather, it is a bit of an up and down “roller coaster.” This helps the patient understand that recovery is not a straight path, there are some ups and downs along the way. An exercise your patient can complete to track their progress is to plot a vertical line where they think they are on this graph at any given time. Over time, they can appreciate their improving function and shrinking experience of pain.
In summary, JCAHO and CMS do not require that you assess pain with a 10 point scale. Achieving zero pain is not the goal. Consider alternate ways of assessing, measuring, and reassessing pain in your patients. Shift the focus from pain to function in order to experience success!
References:
- Bačkonja M “misha”, Farrar JT. Are Pain Ratings Irrelevant? Pain Medicine. 2015;16(7):1247-1250. doi:10.1111/pme.12748
- Ojha HA, Snyder RS, Davenport TE. Direct access compared with referred physical therapy episodes of care: a systematic review. Phys Ther. 2014;94(1):14-30.
- Moseley GL. Reconceptualising pain according to modern pain science. Phys Ther Rev. 2007;12(3):169-178.
- Wilson D, Williams M, Butler D. Language and the pain experience. Physiother Res Int. 2009;14(1):56-65.
- Smart KM, Blake C, Staines A, Thacker M, Doody C. Mechanisms-based classifications of musculoskeletal pain: Part 2 of 3: Symptoms and signs of peripheral neuropathic pain in patients with low back (±leg) pain. Man Ther. 2012;17(4):345-351.
- Smart KM, Blake C, Staines A, Thacker M, Doody C. Mechanisms-based classifications of musculoskeletal pain: Part 3 of 3: Symptoms and signs of nociceptive pain in patients with low back (±leg) pain. Man Ther. 2012;17(4):352-357.
- Smart KM, Blake C, Staines A, Thacker M, Doody C. Mechanisms-based classifications of musculoskeletal pain: Part 1 of 3: Symptoms and signs of central sensitisation in patients with low back (±leg) pain. Man Ther. 2012;17(4):336-344.
- Anson P. AMA drops pain as vital sign. Pain News Netw. 2016. http://accurateclinic.com/wp-content/uploads/2016/04/AMA-Drops-Pain-as-Vital-Sign.pdf.
- Baker DW. Joint Commission statement on pain management. Joint Commission on Accreditation of Healthcare Organizations April. 2016;18:2016.
- Commission J, Others. Pain assessment and management standards for hospitals. Jt Comm J Qual Improv. 2017;11.
- Bates MS, Edwards WT, Anderson KO. Ethnocultural influences on variation in chronic pain perception. Pain. 1993;52(1):101-112.



––– Comments
Sam Ansari
Commented • July 31, 2020
This is a great read. I learnt something new. Thank You. Also, you can check out this. - replayphysio.in
Ina Diener
Commented • July 2, 2020
Very valuable, thanks!