BY: Dr. Jennifer Crane, PT, DPT, OCS, ATC (she/her)
@cirque_physio, www.cirquephysio.com
The spectrum of hypermobility and hypermobility disorders have historically been misunderstood, under-recognized, misdiagnosed, and mismanaged within the medical community. For some patients, hypermobility may not significantly impact their daily lives, but for others, it can be a major source of frustration and an integral part of their identity. When working with hypermobile patients, it’s important to understand the extent of the impact that they have on the patient’s life, as well as the implication of hypermobility on their physical therapy care. This post will discuss what I consider the most critical and often overlooked factors to consider when working with this particular population.
The Spectrum of Hypermobility Disorders
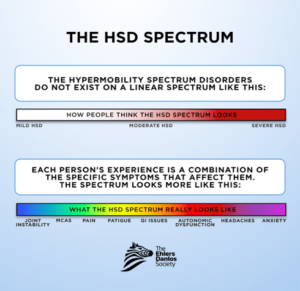
The spectrum of hypermobility is highly complex and non-linear. “Hypermobility” itself is simply a descriptor of joint mobility and is NOT synonymous with “flexibility.” Hypermobility can either be acquired from injury or intentional training, or it can be inherited. It can be symptomatic or asymptomatic and can present with or without other comorbidities. The hypermobility disorders that you’re most likely to encounter clinically are hypermobile-type Ehlers-Danlos syndrome (hEDS) and hypermobility spectrum disorder (HSD). These are both inherited connective tissue disorders, and both are clinical diagnoses of exclusion. Although research is getting quite close, there is not yet a molecular or genetic test available for hEDS or HSD.
Considerations for Clinical Care: Multi-system involvement
One of the most important considerations when treating the hypermobile patient is that they will often have multi-system involvement & comorbidities. Because hEDS and HSD are connective tissue disorders, they impact every system in the body – not just joints. The most common comorbid conditions are:
- Functional GI disorders (gastroparesis, IBS)
- Mast Cell Activation Syndrome (MCAS)
- Dysautonomia:
- Temperature regulatory issues
- Orthostatic intolerance: Postural orthostatic tachycardia syndrom (POTS) & orthostatic hypotension
- Anxiety & depression
- Chronic fatigue
- Migraine & headaches
- Cranio-cervical instability (CCI)
- Neurodiversity: Autism and ADHD
Understanding the systemic impact of these disorders on your patients will dramatically improve efficiency in treatment strategies. Here are a few considerations regarding two of the most common comorbidities: dysautonomia and MCAS
Dysautonomia
Patients with dysautonomia frequently experience symptoms such as dizziness, lightheadedness, and fatigue during physical therapy sessions, which can limit their ability to participate in certain exercises. It is VERY helpful to monitor vitals on these patients, and to allow adequate rest breaks. Exercise prescription during a dysautonomia flare should focus on supine, sidelying, or prone exercises to minimize orthostatic intolerance and prevent symptom exacerbation. These patients also tend to benefit from compression garments and supplemental electrolytes during exercise.
MCAS
MCAS is an immunological condition where mast cells become overly sensitive & overly responsive to various benign triggers, resulting in often severe allergic reactions. Common triggers include temperature changes, certain foods, ANY type of stress, normal hormonal changes, and…exercise. Yes, these patients can (literally) be allergic to exercise if loaded too quickly, so keep that in mind and monitor for beginning signs of allergic reaction and keep antihistamines on hand just in case. Many patients will “pre-game” their physical therapy visits with antihistamines to prevent symptom flares, so don’t be offended if they seem a little groggy during their visit!
Join Dr. Jennifer Crane, PT, DPT, OCS, ATC for April’s Functional Dry Needling Lunch & Learn, happening Tuesday, April 25th from 12:00 – 1:00 PM CT, Register Now!
––– Comments
Dianne Bourque
Commented • April 24, 2023
Thank you for supporting clinical education on hEDS. It is lovely to hear providers with some basic knowledge these days. It means the world to those with this daily challenge.