
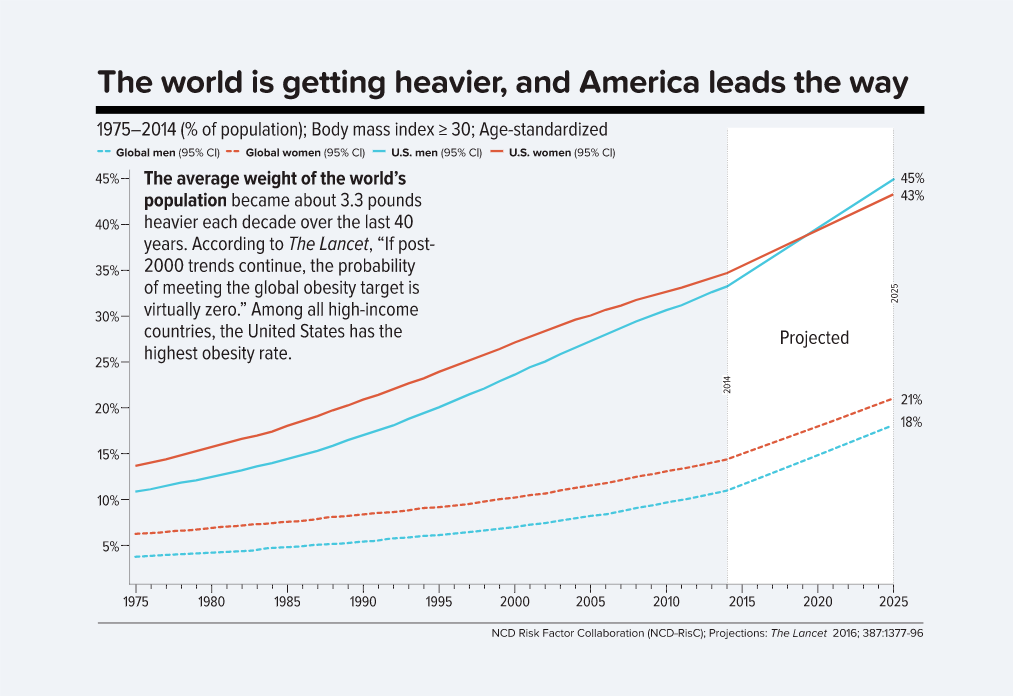
We are well into the summer. The weather is hot, but people are finding ways to get out and enjoy this time of year. We see the pictures on social media of many of our friends and family getting out and moving. Despite this fact, I recently came across an outstanding Harvard Public Health article on obesity in America (thanks for sharing this Mark Milligan). It is amazing to see the trends that are plaguing our country:
The article is a treasure trove of interesting facts about how we got to where we are and what we can do about it. After reading this, it made me start to think about our role as PTs in wellness. Isn’t this one of the hot topics in PT? It needs to be–but are we implementing it effectively?
Regional Interdependence–this term is familiar to many who read this blog. It was a term that made us open our eyes and think more globally about assessment and treatment. Taking a regional approach challenged us to not have tunnel vision. It seems to me that we need to expand the backbone of regional interdependence to a systems mindset. By this I mean we need to look beyond impairments associated with the patient’s chief complaint. We have all assessed a patient with a primary complaint of chronic low back pain, but when we look more global, the patient also has hypertension, diabetes and is a smoker. Although the low back pain is limiting the patient’s ability to function, there are other pressing issues that the PT must address. If not, it would be the same as if we were still using a reasoning model surrounding VMO strengthening for anterior knee pain.
With this being stated, is there a point where we might be thinking too regionally/globally? I know at times when taking in all regional impairments associated with a given patient’s presentation, I could get overwhelmed. Do I address the patient’s poor hip strength, poor patellar mobility or stiff ankle first in this patient with knee pain? Using a sound reasoning process has assisted greatly with this. I had to learn to prioritize–not put the cart before the horse.
I bring this up as I feel the same might be happening in regard to wellness and prevention in PT. I have had some recent conversations with PTs that are doing a great job acknowledging the need to address comorbidities beyond the patient’s primary complaint, but often times are overwhelmed with where to start. Other therapists might utilize outstanding screening intake sheets and processes, but overwhelm the patient with paperwork and assessments on their first day in the clinic.
I think we need to remember to start with small steps. As it stands, we can’t even get PTs in the outpatient setting to consistently take vitals.
And yet we still have to convice many in our profession that #VitalsAreVITAL #ComeOnMan #cvpPT #hypertension #2017NEXT pic.twitter.com/GX1kude7hz
— Rich Severin DPT, PhD(c), CCS (@ptreviewer) June 22, 2017
How many of us are measuring waist circumference? Taking blood pressure and heart rate–not just at intake, but through out a session when appropriate? How many of us are using calculated target heart rates to guide exercise dosage? How about using rating of perceived exertion (RPE) and teaching patients to use this outside the clinic? These components do not need to be done all at initial evaluation, but sprinkled throughout the plan of care. Each little step will lead to the greater intent: promotion of wellness.
Great wellness promotion initiatives and PTs are out there making positive changes: Mike Eisenhart’s #summerofmove and #freetheyoke, Diane Jewell, Jennifer Gamboa and the Body Dynamics crew, and Rich Severn to name a few. It is awesome to see these folks “rallying the masses” to take steps to make wellness promotion something we play a large role in. PTs need to be engaging patients in healthy habits. But, as we look to change behaviors towards improving overall wellness, make sure you are not putting the cart before the horse.
Mark @ShepDPT
